Infection Control in Long-Term Care Facilities: Standards Families Should Ask About
Originally published: August 2025 | Reviewed by Sadie Mays
Originally published: August 2025 | Reviewed by Sadie Mays

When choosing a long-term care facility for someone you love, infection control should be at the top of your checklist.
Long-term care facilities have a higher risk of infection because residents often have weakened immune systems and live in close proximity to one another.
Families can protect their loved ones by asking direct questions about infection control standards, staff training, and outbreak protocols before making this critical decision.
The right questions can reveal whether a facility truly prioritizes infection prevention or if they’re merely checking boxes. Federal regulations now require all long-term care facilities to have dedicated infection prevention programs with trained staff overseeing safety protocols.
Knowing what standards to look for helps families make better choices.
The following guide breaks down the key standards families should evaluate and the specific questions that reveal how well a facility protects its residents.

Long-term care facilities house residents with compromised health who live in close quarters. That creates perfect conditions for infections to spread fast.
Without solid infection prevention protocols, even minor illnesses can turn into serious health threats that affect many residents.
Residents in nursing homes and assisted living facilities face higher infection risks due to their medical conditions and care needs. Many individuals require assistance with basic tasks such as bathing, eating, and taking medications.
This hands-on care means staff members touch residents and their personal items all the time. Without good hand hygiene and equipment cleaning, germs spread easily from person to person.
Residents often have chronic conditions like diabetes, heart disease, or lung problems. These make it harder for their bodies to fight off infections that healthy people might easily shake off.
Common infection risks in long-term care include:
Effective infection prevention and control programs help protect residents by stopping germs before they spread.
As people age, their immune systems get weaker. This process, known as immunosenescence, makes it more challenging for older adults to fight infections.
Older adults also heal more slowly from wounds and illnesses. A cut or cold that heals quickly in a younger person can become a real problem for an elderly resident.
Many residents take multiple medications to manage various health conditions. Some of these medications can weaken the immune system or cause side effects that increase the risk of infection.
Age-related factors that increase infection risk:
Senior care facilities must maintain high infection prevention standards because their residents can’t fight infections as effectively as younger, healthier people.
Long-term care facilities bring many people together in shared spaces. Residents eat meals together, participate in various activities, and utilize common areas such as lounges and therapy rooms.
Bathrooms, dining areas, and medical equipment get used by multiple residents throughout the day. Each shared surface becomes a possible spot for germs to move from one person to another.
Staff members move between different residents’ rooms during their shifts. Without solid infection control, they can accidentally carry germs from room to room on their hands, clothing, or equipment.
High-risk shared areas include:
Visitors can also bring germs into the facility from outside. This includes family, healthcare providers, and delivery workers.
If one resident gets sick, infections can spread rapidly throughout the facility. The 2020 COVID-19 pandemic demonstrated the rapid spread of diseases through nursing homes without proper controls.
Healthcare-associated infections in long-term care settings cause significant illness and death. Outbreaks of flu, norovirus, or other infections can hit dozens of residents within days.
Staff shortages during outbreaks exacerbate the situation. When workers get sick, the remaining staff have to care for more residents, which makes it harder to follow infection prevention steps.
Warning signs of potential outbreaks:
Federal regulations now require long-term care facilities to have infection prevention programs with dedicated staff to monitor and prevent outbreaks before they start.
If you’re ready to get started, call us now!
Hand hygiene serves as the foundation for infection control in long-term care facilities. Personal protective equipment and regular cleaning protocols add extra layers of defense against pathogens that threaten vulnerable residents.
Healthcare workers must wash their hands before and after every interaction with a resident. This simple action removes pathogens that cause infections in vulnerable populations.
Key handwashing moments include:
Staff should use soap and water for at least 20 seconds. Alcohol-based hand sanitizer is effective when soap is unavailable. The facility should put hand sanitizer dispensers at every room entrance.
Residents need help with hand hygiene, too. Staff should assist residents with handwashing before meals and after using the bathroom.
Personal protective equipment acts as a barrier between healthcare workers and infectious pathogens. Staff need to know when and how to use each type of PPE correctly.
Gloves are required when:
Gowns protect clothing during messy procedures. Workers wear them when splashing is likely or when caring for residents with certain infections.
Masks prevent respiratory droplets from spreading. Staff put on masks when residents have coughs, colds, or respiratory infections. Some places require masks during flu season or outbreaks.
Workers must put on PPE in the correct order and remove it carefully to prevent contamination. It’s not always easy, but it’s necessary.
Cleaning and disinfecting remove pathogens from surfaces that people touch a lot. These areas can harbor germs that spread from person to person throughout the day.
High-touch surfaces requiring daily cleaning:
Staff should clean surfaces with soap first to get rid of dirt. Then they use EPA-approved disinfectants to kill leftover germs.
The facility should increase cleaning during outbreaks. Some areas may need cleaning several times a day. Staff rooms, elevators, and common areas also require regular attention to prevent the spread of germs.
Long-term care facilities must have clear plans for keeping sick residents away from healthy ones.
Staff assignments are adjusted during outbreaks to prevent the spread between units, and families receive regular updates on their loved ones’ safety.
Facilities should have designated areas to house residents with contagious infections. Single rooms are best suited for isolating residents with respiratory viral infections, such as influenza or pneumonia.
Some infections need different types of isolation:
Contact Precautions:
Droplet Precautions:
Standard Precautions:
Facilities may use entire wings or floors during large outbreaks. This helps contain diseases like Clostridioides difficile that spread easily through contact with contaminated surfaces.
The facility should clearly explain which residents require isolation and provide justification for this decision. They should also inform families of the expected duration of isolation, based on the specific infection.
During outbreaks, facilities assign certain staff to work only in infected areas. This helps prevent germs from spreading between healthy and sick areas.
These workers don’t cover other parts of the building during their shifts. Whenever possible, they use different entrances and stick to strict handwashing routines.
The infection prevention program calls for enough staff to care for residents in isolation. Families might want to ask if the facility has backup plans for staffing during outbreaks.
Staff receive additional training on the use of protective gear. They practice putting on and taking off gowns, gloves, and masks to prevent the spread of infections.
Facilities notify families within 24 hours when an outbreak starts. They explain what kind of infection is spreading and which sections are affected.
Regular updates keep families in the loop about their loved one’s health. The facility should provide:
Some places restrict or pause visits during severe outbreaks. They usually offer video calls or other ways for families to stay in touch with residents.
The outbreak management guidance requires facilities to report certain infections to health departments. Families have a right to know about these reports and what steps officials are taking.
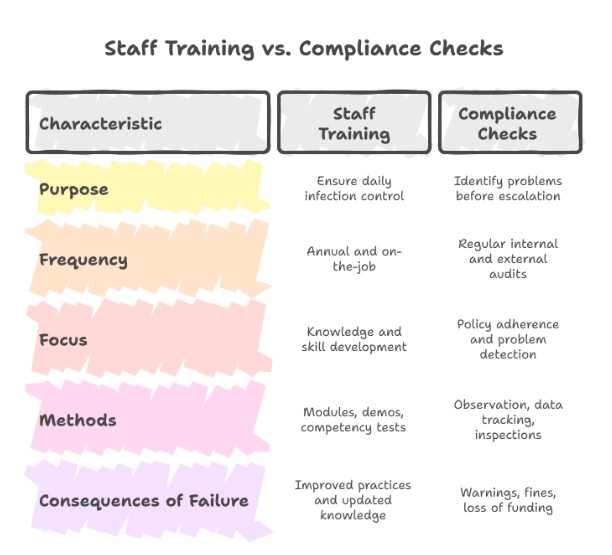
Consistent staff training ensures infection control is followed daily, not just during inspections.
Staff training programs help employees learn and follow current infection control practices.
Regular compliance checks enable facilities to identify problems before they escalate into larger issues.
Long-term care facilities provide specialized training in infection prevention and control to staff before they begin their jobs. This training covers basic topics such as hand hygiene, isolation procedures, and the use of personal protective equipment.
Staff receive ongoing education to stay current with the latest guidelines from the CDC and other health organizations. Topics include preventing HAIs, antibiotic stewardship, and outbreak response procedures.
Key Training Areas:
New hires complete infection control training within their first 30 days. Experienced staff take annual refresher courses and get updates when guidelines change.
Facilities utilize online modules, hands-on demonstrations, and competency tests to ensure staff understand the material. Some require staff to pass written exams before working with residents.
Internal audits enable facilities to verify that staff adhere to infection control policies. These typically occur monthly or quarterly and encompass every department.
Infection preventionists watch staff during daily tasks to spot gaps in compliance. They look at hand hygiene, equipment use, and documentation.
Common Audit Areas:
External surveyors from state health departments do annual inspections. The CMS Quality, Safety, and Education Portal trains these surveyors for consistent evaluations.
Facilities track healthcare-associated infections and report trends to staff and providers. This data helps them identify areas that require additional training or policy changes.
Facilities that fail to meet infection control standards are facing increasing penalties from regulators. First violations usually bring warnings and a corrective action plan.
Repeat violations can result in fines ranging from hundreds to thousands of dollars per day. Serious violations might result in temporary admission restrictions or loss of Medicare and Medicaid funding.
Progressive Penalties:
State health departments can revoke facility licenses for ongoing failures in infection control. This typically occurs only when facilities fail to address serious problems over time.
Families should inquire about recent inspection results and any corrective actions that have been taken. Public databases post inspection reports and violation histories for most long-term care facilities.
Sadie G. Mays Health & Rehabilitation Center combines quality Rehabilitation services with strict infection control standards. Discover how our therapies promote a safe recovery—contact us now to schedule your consultation.
If you’re ready to get started, call us now!
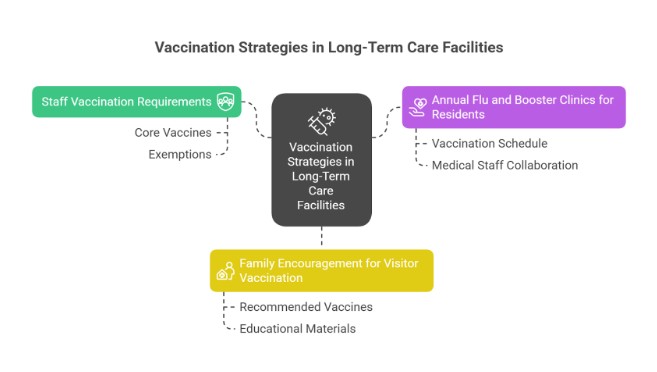
Vaccines help prevent flu, COVID-19, and pneumonia outbreaks in long-term care settings.
Vaccination against respiratory diseases, such as influenza, pneumococcal disease, pertussis, and COVID-19, is a simple and effective way to reduce the infection burden in care facilities.
Long-term care facilities keep strict vaccination policies for employees. Staff immunizations help prevent the transmission of germs to residents and reduce missed workdays.
Most places require these core vaccines for staff:
Staff usually can’t work without proof of required vaccinations. Some facilities allow medical or religious exemptions, but add extra safety steps.
New hires complete vaccine requirements during orientation. Facilities should cover the cost of staff vaccines.
Care facilities hold vaccination clinics to ensure residents receive timely immunizations. These clinics make vaccines easily accessible without requiring outside appointments.
Typical vaccination schedule for residents:
| Vaccine Type | Frequency | Timing |
| Influenza | Annual | September-October |
| COVID-19 boosters | As recommended | Updated seasonally |
| Pneumococcal | One-time or series | Upon admission |
| Shingles (Zoster) | Two doses | Ages 50+ |
The medical staff collaborates with residents’ doctors to determine which vaccines are necessary. They check each resident’s health and vaccine history.
Clinics are held in common areas or residents’ rooms. Licensed nurses give the shots and watch for any immediate reactions.
Families get advance notice about upcoming clinics. The facility receives consent from residents or their healthcare decision-makers before giving any vaccines.
Facilities encourage families and visitors to stay up to date with their vaccines. This adds another layer of protection for residents who might have weaker immune systems.
Recommended vaccines for regular visitors include:
Some places check vaccination status at the door. Others distribute educational materials explaining why visitor immunization is important.
Families should tell the facility if they’re feeling sick before visiting. Even vaccinated individuals can occasionally transmit germs to residents.
The facility might restrict visits from unvaccinated people during outbreaks. These steps help protect everyone when infection risks spike in the community.
Families should ask how facilities handle infection prevention, outbreak reporting, and resident safety.
When touring long-term care facilities, families should ask about infection control training, outbreak policies, and inspection records.
These areas indicate how effectively a facility safeguards residents from preventable infections.
Staff training frequency is crucial for resident safety. Facilities should conduct staff training during orientation and provide ongoing sessions throughout the year.
Ask about the training schedule. Good facilities run infection control training at least every quarter. Some offer monthly updates or extra sessions during flu season.
Find out what topics the training covers:
Find out who teaches the training. Long-term care facilities should have infection prevention programs led by qualified staff or outside experts.
Ask if the facility tracks who completes training. Good facilities maintain records showing which staff members have completed training and when. They usually test staff knowledge to ensure everyone understands it.
Outbreak response policies show if a facility is really ready for infectious emergencies. Every place should have written plans for different types of outbreaks.
Ask to see their outbreak plan. It should spell out steps for identifying cases, notifying health authorities, and protecting other residents.
Key parts of a solid outbreak policy include:
Ask how quickly they implemented restrictions. Facilities should act within hours, not wait for days.
Ask about testing. Skilled nursing facilities have strengthened their infection prevention programs since the COVID-19 pandemic, including the implementation of access to rapid testing.
Inspection reports reveal how a facility actually performs in terms of infection control and safety. These reports are publicly available, allowing families to review them at any time.
Most facilities display their latest inspection report in a visible location. When you visit, ask to see both the state health department’s inspection report and the federal survey results.
Look for these infection control issues in reports:
Check how the facility responded to any violations. The best places act fast and put real effort into fixing problems.
When touring facilities, families should ask about staff response protocols and safety measures. It’s good to know how the facility handled past outbreaks or infection control challenges.
Ask to see follow-up inspection reports, too. These reports show whether the facility actually corrected problems or if the same issues kept coming up.
Families can review inspection records through Georgia HFRD and CMS Care Compare. You can dig into detailed inspection records through government databases. These enable you to track how well a facility adheres to infection control standards.
The records reveal citation patterns, helping you identify facilities with recurring problems. It’s a bit of homework, but it’s worth it.
The Health Facilities Reporting Database (HFRD) offers thorough inspection histories for nursing homes and long-term care facilities. Just search by name or location to find detailed reports.
The database lists infection control violations with dates and severity. Each citation spells out what inspectors found and what the facility’s supposed to do about it.
Recent inspections matter most. If you look at patterns from the last couple of years, you’ll get a clearer picture.
Key information to review:
You can filter by violation type in the search. Focus on categories like “infection prevention” and “sanitation”—that’s where the real story is.
The Centers for Medicare and Medicaid Services gives star ratings from one to five for health inspections. Infection control and safety play a big role in these ratings.
If a facility has three stars or higher, it usually meets acceptable infection control standards. Two stars or less? That’s a red flag, and you’ll want to look deeper.
They base ratings on both the number and seriousness of violations. Even one major infection control issue can quickly drop a rating.
Rating breakdown:
CMS updates these ratings monthly, ensuring you have access to the latest inspection data.
When inspectors cite a facility for the same infection control issue more than once, it typically indicates systemic problems. It’s rarely just a one-off mistake; usually, it’s a sign that management isn’t paying close enough attention or staff training isn’t up to par.
What are the most common repeat violations? Improper hand hygiene, sloppy isolation procedures, and failure to report outbreaks. If a facility racks up the same citation three or more times in two years, that’s a huge compliance red flag.
Warning signs to avoid:
Inspectors now use updated infection control assessment tools to identify these patterns more quickly.
If I were choosing a facility, I’d look for one with a clean inspection record rather than one with a string of repeated violations.
Choose Sadie G. Mays Health & Rehabilitation Center for reliable, compassionate Long-Term Care backed by proven infection prevention. Protect your loved one’s health—contact us today to schedule a tour.
If you’re ready to get started, call us now!
What is infection control in long-term care?
Infection control is a set of practices that prevent the spread of illnesses among residents, staff, and visitors in shared care environments.
How often are facilities inspected for infection control?
Georgia facilities are inspected annually by HFRD and CMS, with additional unannounced visits if complaints or safety concerns are reported.
What infections are most common in long-term care facilities?
Respiratory infections, urinary tract infections, skin infections, and gastrointestinal illnesses are the most frequently reported.
How can families review a facility’s infection control history?
Families can access public inspection reports through the Georgia HFRD database and Medicare’s CMS Care Compare tool.
What role do vaccines play in infection prevention?
Vaccination programs for residents and staff reduce outbreaks of flu, COVID-19, and pneumonia, protecting high-risk populations.
What should families ask during a tour about infection control?
Questions to ask include: “How often are staff trained?” and “What’s your plan if there’s a flu or COVID-19 outbreak?”
Can visitors impact infection control in long-term care?
Yes. Visitors are often asked to follow mask, hand hygiene, and screening policies to protect residents from preventable illnesses.