Hospital Discharge Planner Guide: Requesting Preferred SNF Placement in Atlanta
Originally published: October 2025 | Reviewed by Sadie Mays
Originally published: October 2025 | Reviewed by Sadie Mays

Discharging a patient from a hospital to a skilled nursing facility can feel overwhelming. Patients and families often have strong preferences about where they want to receive care.
In Atlanta’s healthcare system, discharge planners work closely with patients to coordinate transfers to appropriate skilled nursing facilities.
But wow, this process really demands clear communication and a solid grasp of the available options.
Patients and their families can request preferred skilled nursing facilities during discharge planning. Final placement depends on factors such as bed availability, insurance, and whether the facility can adequately address the patient’s specific medical needs.
The hospital discharge planning process centers on patient goals and treatment preferences. Planners involve patients and caregivers as active partners, not just bystanders.
Knowing how to communicate with discharge planners and what information to have ready can significantly increase your chances of securing a spot at your preferred facility.
If you understand what SNFs look for and how to navigate Atlanta’s competitive placement scene, the whole process becomes less stressful.

Hospital discharge planners in Atlanta guide patient transitions from acute care to skilled nursing facilities. They initiate the process at admission and maintain a set timeline to ensure a safe transfer.
Discharge planners look at medical, physical, psychological, and social needs before making SNF arrangements.
They review diagnoses and current conditions and determine the level of care the patient needs to select the right facility.
Assessment responsibilities include:
The planner collaborates with numerous individuals along the way. They discuss medical orders and treatment plans with doctors, and social workers help identify potential barriers.
Coordination activities involve:
Planners also handle a ton of paperwork. They manage forms and ensure that all the information gets where it needs to go.
They complete referral forms, gather medical records, and submit insurance authorizations to ensure everything is on track.
The discharge planning process starts at admission and continues throughout the hospital stay. Planners work with utilization review to monitor patient progress and predict discharge needs.
Once the discharge decision is made, things move quickly. Planners often have just 24-48 hours to find an SNF bed after doctors give the green light.
Atlanta’s SNF market can get competitive. Planners typically reach out to multiple facilities simultaneously to secure a spot quickly.
If you’re ready to get started, call us now!
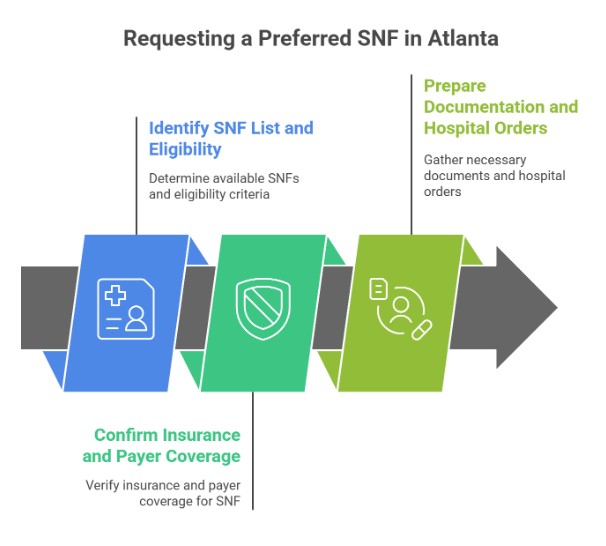
If you want a specific SNF, you’ll need to identify eligible facilities, check insurance, and get your paperwork in order. This means working with the hospital team, insurance, and your chosen SNF.
Discharge planners should pull the insurance-approved SNF list for Atlanta. Each insurance plan works with different facilities.
Medicare requires a minimum three-day inpatient hospital stay for SNF coverage.
Key eligibility requirements include:
Planners must check that the patient meets Medicare’s criteria for skilled care. This typically involves tasks such as wound care, IV administration, or physical therapy that require the expertise of licensed nurses.
Patients in Atlanta should prefer in-network facilities whenever possible. Out-of-network SNFs cost more and can be a headache to get approved.
The planner contacts preferred facilities to see who has beds available. Sometimes, especially during busy periods, you’ll need backup options.
Verifying insurance up front saves a lot of trouble later. Planners confirm active coverage and the details before making requests.
Coverage verification includes:
Most Medicare Advantage and commercial plans want prior authorization before SNF admission. Every insurance company does this a little differently.
Some insurers grant auto-approval for 5 days after reviewing benefits and medical necessity. Others want a full review first.
Planners should call the insurance case management department directly. That way, you get the most accurate info and catch any special requirements for your chosen SNF.
Solid documentation is key for SNF requests. Missing paperwork can slow down the process or even result in denials.
Required documentation includes:
The attending doctor needs to write specific orders for skilled services. Vague orders, such as “SNF placement,” usually don’t suffice for insurance approval.
Planners should add functional assessments and safety concerns to the request. This helps show why 24-hour skilled nursing is necessary.
All forms need the correct patient info and insurance details. Many insurance portals now allow you to submit SNF admission forms online.
Patient Information:
Medical Documentation:
Insurance Requirements:
Facility Coordination:
Sadie G. Mays helps discharge planners and families secure preferred SNF placements quickly by coordinating insurance, records, and bed availability. Schedule an appointment now.
If you’re ready to get started, call us now!
Skilled nursing facilities in Atlanta consider several factors before accepting hospital transfers. Clinical care needs, insurance coverage, and bed space all play a part.
SNFs only accept patients who require skilled nursing or rehabilitation services that can’t be provided at home. Medical necessity requirements must be met for coverage.
Facilities review each patient’s records to confirm whether skilled services are required daily. The patient requires professional nursing or therapy services, not just basic assistance.
Some SNFs focus on certain conditions. Cardiac centers care for heart patients, while orthopedic SNFs handle joint replacements and similar procedures.
Insurance coverage plays a big role in whether an SNF will accept a patient. Medicare, for example, requires a three-day hospital stay before it’ll cover the cost. Updates to SNF coverage in 2025 might shake up these requirements.
Key Insurance Factors:
Bed availability can totally change the admission timeline. Popular places usually have waiting lists, sometimes long ones.
Some facilities save beds for their partner hospitals. That can leave others waiting even longer.
Before letting someone in, facilities check your finances. They’ll confirm insurance benefits and coverage limits, and some insurers want prior authorization before you move in.
| Payer Type | Requirements | Notes |
| Medicare | 3-day hospital stay + skilled need | Advantage plans may need prior authorization |
| Medicaid | State-based rules vary by facility | Not all Atlanta SNFs accept |
| Private | Contract-based limits | Often caps at 20–30 days |
| Self-Pay | N/A | Still depends on bed availability |
Atlanta hospitals usually have their own preferred SNF networks. These partnerships can significantly accelerate the care transition process and enhance patient outcomes.
Major Atlanta systems, such as Emory University Hospital, Piedmont Atlanta, and Grady Memorial, maintain strong SNF referral networks that can influence bed access.
Partnership Benefits Include:
Major hospital systems maintain close ties with SNFs. Their patients often get priority for open beds.
Smaller hospitals might have fewer partnership options. These relationships can significantly impact the speed at which patients are placed.
Partnerships aren’t just about convenience. Hospitals track readmission rates from their SNF partners. If a facility’s numbers slip, referrals might drop off.
Most Atlanta SNFs adhere to standard admission rules that extend beyond insurance or clinical needs. Age, behavior, and the level of family involvement can all tip the scales.
| Admission Requirement | What It Means | Notes |
| Medically stable | No acute hospital-level needs | Required for all SNFs |
| Skilled need | Daily therapy or nursing services | Wound care, IVs, rehab |
| Insurance coverage | Approved payer or self-pay | Medicare, Medicaid, or private |
| Family support | Ability to participate in care planning | Improves outcomes |
Some places have specialty units. Memory care units take dementia patients, while ventilator units handle more challenging respiratory cases.
Location matters, too. Facilities consider how close families are when determining whether beds are available. Good transportation options can significantly impact long-term success.
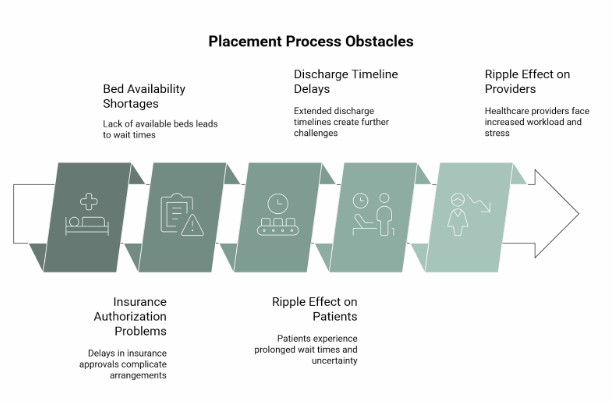
Discharge planners in Atlanta face three significant challenges: limited bed availability, delays in insurance authorization, and lengthy discharge timelines.
Proactive measures, such as holding beds early, maintaining backup lists, and arranging transportation in advance, can significantly alleviate stress.
Atlanta SNFs usually run at 85-90% capacity. The most popular spots may require you to wait two or three weeks for a bed.
Specialty units, such as those for ventilator or bariatric care, have even longer wait times.
Discharge planners often end up competing with each other for the same beds, especially on weekdays when the best facilities fill up quickly.
Medicare Advantage plans often ask for prior authorization before covering SNF stays. That can take three to five business days, sometimes longer.
Patients waiting for Medicaid approval face additional challenges, as not every facility accepts them.
Private insurance typically limits SNF coverage to 20-30 days, and some plans prioritize lower levels of care initially.
Team dynamics in discharge planning can significantly slow down the process. Doctors might change orders at the last minute, affecting what level of care a patient needs.
Families sometimes delay the decision, especially if multiple relatives need to sign off. Weekend discharges rarely go smoothly since administrative staff are thin on the ground.
If you’re ready to get started, call us now!
Grab the bed holds within a day or two of spotting the SNF need. Most places allow you to hold a bed for three to five days if you have the necessary paperwork.
Send clinical summaries and insurance information as soon as you request the hold. Case management assistants track logistics and maintain open communication with facilities. Checking the hold status daily helps avoid losing the spot.
Keep up-to-date relationships with 8-10 SNFs across Atlanta. Ensure your list encompasses various insurance types and patient needs.
Having direct phone numbers for admission coordinators saves headaches. Rank facilities by the odds they’ll accept your patient, but sometimes you just have to go with whoever has a bed.
Book medical transport at least a day before discharge. Double-check with the SNF to determine if the patient requires a wheelchair or stretcher, and arrange for oxygen or IV pumps as necessary.
Try to match the discharge with SNF admission staff schedules. Most places prefer arrivals in the afternoon, usually between 1 and 4 PM, so orientation doesn’t get rushed.
Selecting the right skilled nursing facility can significantly impact recovery and readmission rates.
Facility quality ratings, therapy programs, and staffing levels all contribute to how well someone transitions from the hospital to home.
Studies show that the hospital discharge planning experience really shapes recovery outcomes. If you land in the wrong facility, you’re more likely to get readmitted or take longer to bounce back.
Facilities with enough staff tend to get better results. When patients get skilled care that matches their needs, they recover faster than those who don’t.
Hospital discharge planners assess medical complexity to determine whether someone needs an SNF. The assessment sets the tone for the level of care required.
Key Research Findings:
Nursing home quality indicators in Georgia help families evaluate facilities. Review staffing, safety, and outcome data to gain insight into the current situation.
Critical Quality Factors:
| Factor | What to Check |
| Staffing Ratios | Registered nurse hours per patient day |
| Therapy Programs | PT/OT/ST availability and intensity |
| Safety Records | Infection rates and incident reports |
| Outcomes | Discharge to home rates and readmission data |
Skilled nursing facilities provide both medical care and rehabilitation services. The key is finding a location that aligns with the patient’s medical needs and goals.
Therapy intensity varies from one setting to another. Patients typically require daily skilled care from nursing or therapy staff to qualify for a SNF placement.
Sadie G. Mays Health & Rehabilitation Center in Atlanta stands out for its specialized skilled nursing services. They focus on smooth post-acute transitions and strong rehabilitation outcomes.
The center’s comprehensive long-term care services bridge the gap between skilled nursing and traditional nursing home care. That kind of flexibility can really help patients with changing needs.
Sadie G. Mays Advantages:
Discharge coordinators at Sadie G. Mays work side-by-side with hospital planners. This teamwork helps smooth out transitions and reduces the risk of complications or readmissions.
Securing your preferred skilled nursing facility placement in Atlanta requires engaging in discharge planning early.
Patients and families should clearly communicate their preferences to hospital discharge planners from the outset.
Key Actions for Success:
The hospital discharge planning process involves a comprehensive team effort. You have a say here—patients can ask for specific facilities.
Documentation matters. If you want your preferred placement, keep track of every request and all your communications with the discharge team.
Hospitals must follow federal discharge planning requirements (Medicare.gov Checklist).
| Payer Type | Requirements | Notes |
| Medicare | 3-day stay + skilled need | Advantage plans may require prior authorization |
| Medicaid | Varies by state | Not all Atlanta SNFs accept |
| Private | Depends on the contract | Often limited to 20–30 days |
| Self-Pay | N/A | Bed availability is still required |
Choosing the right SNF after hospitalization is critical. Sadie G. Mays offers trusted care, smooth admissions, and family support. Contact us today to get started.
What is the role of a hospital discharge planner in Atlanta?
A discharge planner coordinates patient transitions from the hospital to post-acute care, ensuring that insurance approval, medical record transfer, and family preferences are respected.
How can families request a preferred skilled nursing facility (SNF) during discharge?
Families should tell the discharge planner their preferred SNF early, verify bed availability, and provide necessary insurance and documentation to secure placement.
What documents are needed for SNF admission from a hospital?
Hospitals typically provide a discharge summary, medication list, therapy orders, recent lab results, and insurance authorization for SNF transfer approval.
How do skilled nursing facilities decide whether to accept a patient transfer?
SNFs evaluate clinical needs, payer source, and bed availability. They also review hospital documentation to ensure they can meet the patient’s care plan.
What are common obstacles to securing preferred SNF placement in Atlanta?
Challenges include bed shortages, insurance denials, last-minute discharge decisions, and transportation delays. Early planning with the discharge team helps overcome them.
Why does choosing the right SNF matter for hospital patients?
The right SNF reduces hospital readmissions, improves rehabilitation outcomes, and offers families peace of mind during recovery and long-term care.
How can families in Atlanta prepare for smoother SNF placement?
Start discussions early, tour potential facilities, confirm insurance coverage, and maintain open communication with the hospital’s discharge planning team.